-
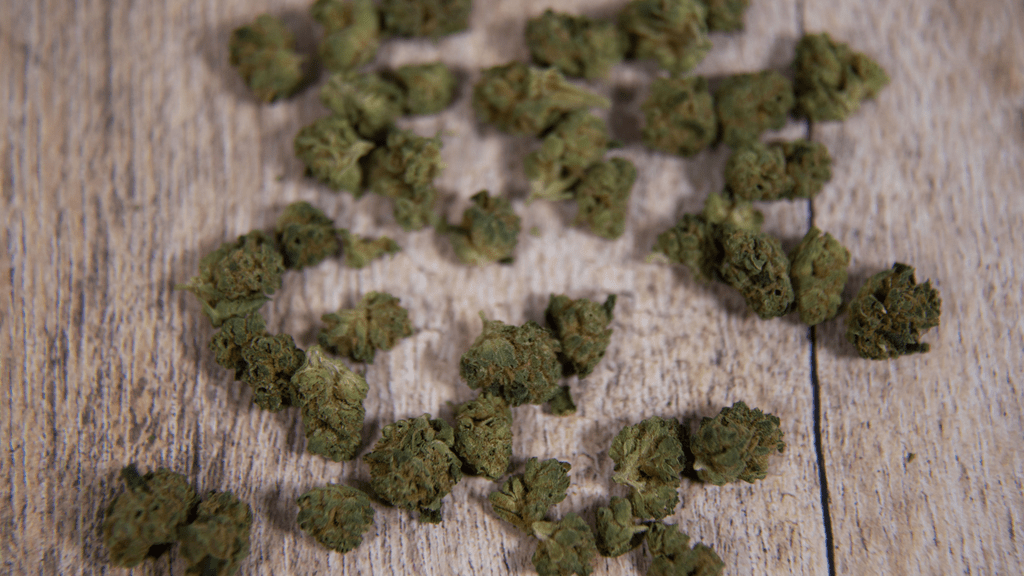
Cannabis and Opioid Use: A New Perspective from Medical Studies
Read more: Cannabis and Opioid Use: A New Perspective from Medical StudiesIn recent years, the conversation surrounding the medical use of cannabis has taken a significant turn, with numerous studies shedding light on its potential benefits,…